Today, the world’s population of seniors is at an all-time high. Families, communities, and governments face daunting challenges as they scramble to keep up. Seniors themselves can benefit from becoming aware of the many problems that need to be solved in order to produce not only an acceptable quality of life, but a life enriched by resources and activities that can be structured to give the elderly the maximum benefits of a life well lived. This section will highlight problems and offer solutions based on the latest senior living studies.
The top ten concerns facing senior citizens today include:
1. Health Care Costs – The older we get, the more healthcare we need. It is important to get screenings for disease and natural aging conditions to catch any health issues in their beginning stages. While doctor visits multiply, medical costs are rising, which can impact one’s retirement budget.
"Great product, great service, what more can I say?"
 5. Financial Security – The rising cost of living while living on a fixed income poses new financial restrictions. We may not be able to afford the same comforts of life that we used to.
5. Financial Security – The rising cost of living while living on a fixed income poses new financial restrictions. We may not be able to afford the same comforts of life that we used to.
This is paragraph text. Double click here to edit and add your own text.
6. Loneliness – Getting older means that our friends are aging, as
well. It is common for seniors to lose their friends to Alzheimer’s
disease or even death. Spending time with remaining friends and
family members becomes all the more important. A pet can be
wonderful for daily companionship, as well.
 7. Financial Predators – Sadly, it is a fact that there are unscrupulous people looking to prey on senior citizens. They will try to sell unnecessary goods or services to those they see as vulnerable. Share your financial decisions with someone you trust. A financial advisor may be necessary, but most of us have at least one friend or family member willing to offer free advice.
7. Financial Predators – Sadly, it is a fact that there are unscrupulous people looking to prey on senior citizens. They will try to sell unnecessary goods or services to those they see as vulnerable. Share your financial decisions with someone you trust. A financial advisor may be necessary, but most of us have at least one friend or family member willing to offer free advice.
This is paragraph text. Double click here to edit and add your own text.
8. Abuse or Neglect – Nursing homes and assisted living facilities struggle with under-staffing issues, which can lead to abuse or neglect of the residents. Be sure to find a place to live that comes highly recommended by people you trust.
 9. Transportation – Our reflexes can slow as we age and our eyes can become less clear. This may lead us to give up driving for our safety and the safety of others. Thankfully, transportation is available specifically for those who need it, including seniors.
9. Transportation – Our reflexes can slow as we age and our eyes can become less clear. This may lead us to give up driving for our safety and the safety of others. Thankfully, transportation is available specifically for those who need it, including seniors.
This is paragraph text. Double click here to edit and add your own text.
10. Changing social climate – Adjusting to technological changes is probably the largest social hurdle we can face as senior citizens. See your local library for free classes on using computers.
To address these growing concerns for seniors everywhere, we have included a group of articles below, that showcase initiatives that are meeting these challenges, and encouraging support for elder concerns.
Health insurance for senior citizens in the Philippines may be availed of
in 2 ways.
1. By becoming a member of Philhealth or the Philippine Health
Insurance Corporation. It is a government owned and controlled
corporation.
2. By buying a health insurance policy from a private health insurance
company.
There are 30 licensed private life insurance companies in the
Philippines offering various health insurance products.
But before looking for a private insurance product, please be aware that there
is a Philippine Law that provides for mandatory PhilHealth
coverage for all senior citizens. Premium payments are subsidized by
the Philippine government. This means that senior citizens will receive the benefits and discounts extended to ordinary PhilHealth members by just presenting a valid ID
that proves their real age.
For convenience, senior citizens may go to the nearest DSWD office and
apply for a senior citizen ID card. It is free. Sometimes though, Philhealth benefits will not fully cover all the bills of a costly hospitalization, "Health Support Hospital
Income Plan" sold by Philippine Prudential Life Insurance is available if you are a senior citizen aged between 50 and 74. Acceptance into this Plan, without medical examination nor complicated health questions to answer, is guaranteed.
Take this for an example, you are a senior citizen aged 64. You bought
a health insurance product mentioned above. For a monthly premium of
P287.95, you will be entitled to the following benefits.
1. Daily hospital income benefit of P500 if you get hospitalized.'
Maximum limit is P91,250
2. Daily critical care benefit of P500
Maximum limit is P91,250
3. Surgical benefit
Maximum limit is P10,000
The example cited above is the lowest benefit plan. You may opt for a
higher plan if you want to avail of a higher benefit amount.
Australian researchers have come up with a non-invasive ultrasound technology that clears the brain of neurotoxic amyloid plaques - structures that are responsible for memory loss and a decline in cognitive function in Alzheimer’s patients. If a person has Alzheimer’s disease, it’s usually the result of a build-up of two types of lesions - amyloid plaques, and neurofibrillary tangles. Amyloid plaques sit between the neurons and end up as dense clusters of beta-amyloid molecules, a sticky type of protein that clumps together and forms plaques.
Neurofibrillary tangles are found inside the neurons of the brain, and they’re caused by defective tau proteins that clump up into a thick, insoluble mass. This causes tiny filaments called microtubules to get all twisted, which disrupts the transportation of essential materials such as nutrients and organelles along them, just like when you twist up the vacuum cleaner tube. As we don’t have any kind of vaccine or preventative measure for Alzheimer’s - a disease that affects 343,000 people in Australia, and 50 million worldwide - it’s been a race to figure out how best to treat it, starting with how to clear the build-up of defective beta-amyloid and tau proteins from a patient’s brain. Now a team from the Queensland Brain Institute (QBI) at the University of Queensland have come up with a pretty promising solution for removing the former.
Therapeutic Ultrasound
Publishing in Science Translational Medicine, the team describes the technique as using a particular type of ultrasound called a focused therapeutic ultrasound, which non-invasively beams sound waves into the brain tissue. By oscillating super-fast, these sound waves are able to gently open up the blood-brain barrier, which is a layer that protects the brain against bacteria, and stimulate the brain’s microglial cells to activate. Microglial cells are basically waste-removal cells, so they’re able to clear out the toxic beta-amyloid clumps that are responsible for the worst symptoms of Alzheimer’s.
The team reports fully restoring the memory function of 75 percent of the mice they tested it on, with zero damage to the surrounding brain tissue. They found that the treated mice displayed improved performance in three memory tasks - a maze, a test to get them to recognize new objects, and one to get them to remember the places they should avoid. "We’re extremely excited by this innovation of treating Alzheimer’s without using drug therapeutics," one of the team, Jürgen Götz, said in a press release. "The word ‘breakthrough’ is often misused, but in this case I think this really does fundamentally change our understanding of how to treat this disease, and I foresee a great future for this approach."
The team says they’re planning on starting trials with higher animal models, such as sheep, and hope to get their human trials underway in 2017.
Getting adequate nutrition can be a challenge as you get older. With age, the number of calories you need begins to decline. Every calorie you consume must be packed with nutrition in order to hit the mark.
Even then, you may fall short. "As we get older, the body becomes less efficient at absorbing some key nutrients," says Katherine Tucker, RD, PhD, chair of the department of health sciences at Northeastern University in Boston. In addition, the ability to taste food declines, blunting appetite. Some foods become difficult to chew or digest.
Several key nutrients in particular may be in short supply as you get older. Here are the top vitamins and nutrients to look out for -- and how to get enough.
Vitamin B12
B12 is important for creating red blood cells and DNA, and for maintaining healthy nerve function. “Getting enough B12 is a challenge for older people because they can’t absorb it from food as well as younger people," says Tucker. "Even if your diet contains enough, you may be falling short."
How to hit the mark: Eat more foods rich in B12. The richest sources include fish, meat, poultry, eggs, milk, and milk products. Talk to your doctor about whether you should take a B12 supplement.
Folate/Folic Acid
You may have heard of folate. Too little of this essential B vitamin is known for contributing to anemia and increasing the risk of a pregnant woman having a baby with a neural tube defect. Older people whose diets don’t include a lot of fruits and vegetables or fortified breakfast cereals may be falling short.
How to hit the mark: Now that breakfast cereals are fortified with folate, deficiencies are less common. "Still, if you don’t eat breakfast cereals or plenty of fruits and vegetables, it’s wise to ask your doctor if you should take a supplement that contains folate," says Kathleen Zelman, RD, director of nutrition for WebMD.
Calcium
Calcium plays many roles in the body. But it is most important for building and maintaining strong bones. Unfortunately, surveys show that as we age, we consume less calcium in our diets. "Calcium is so essential that if you don’t get enough, your body will leach it out of your bones," says Zelman. Coming up short on calcium has been shown to increase the risk of brittle bones and fractures.
How to hit the mark: Help yourself to three servings a day of low-fat milk and other dairy products. Other good dietary sources of calcium include kale and broccoli, as well as juices fortified with calcium. Calcium-rich foods are by far that best choice, says Robert Heaney, MD, a Creighton University professor of medicine and an expert on calcium and vitamin D. "The body needs both calcium and protein for bone health," says Heaney. "So the ideal source of calcium is dairy products, not supplements." If you tend to steer clear of dairy products, talk to your doctor about whether you should take a supplement.
 Vitamin D
Vitamin D
"Vitamin D helps the body absorb calcium, maintain bone density, and prevent osteoporosis," says Zelman. Recent findings suggest that D may also protect against some chronic diseases, including cancer, type 1 diabetes, rheumatoid arthritis, multiple sclerosis, and autoimmune diseases. In older people, vitamin D deficiency has also been linked to increased risk of falling. Many Americans fall short on vitamin D, which is mainly produced by the skin when exposed to sunlight.
This is paragraph text. Double click here to edit and add your own text.
Potassium
Getting enough potassium in your diet may also help keep bones strong. This essential mineral is vital for cell function and has also been shown to help reduce high blood pressure and the risk of kidney stones. Unfortunately, surveys show that many older Americans don’t get the recommended 4,700 mg of potassium a day.
How to hit the mark: Fruits and vegetables are by far the richest dietary sources of potassium. Banana, prunes, plums, and potatoes with their skin are particularly rich in potassium. By helping yourself to fruits and vegetables at every meal, you can get enough potassium. If you’re considering potassium supplements, talk to your doctor first. Just as too little potassium can be a problem, too much potassium can be very dangerous for your health.
Magnesium
Magnesium plays a crucial role in some 300 different physiological processes. Getting enough can help keep your immune system in top shape, your heart healthy, and your bones strong. "Many whole foods, including vegetables, contain magnesium. But it is often lost in processing," says Tucker. Absorption of magnesium decreases with age. Some medications older people take, including diuretics, may also reduce magnesium absorption.
How to hit the mark: Fill your plate with as many unprocessed foods as possible, including fresh fruits, vegetables, nuts, whole grains, beans and seeds, all of which are great sources of magnesium.
Fiber
Fiber helps promote healthy digestion by moving foods through the digestive tract. Foods rich in fiber, including whole grains, beans, fruits, and vegetables, have many other health benefits, including protecting against heart disease. "If you don’t eat a lot of these whole foods, chances are you’re not getting enough fiber," says Zelman. You’re not alone. Most Americans only get about half the recommended levels.
How to hit the mark: Eat more whole grains, nuts, beans, fruits, and vegetables. Be creative. "Try adding cranberry sauce to your turkey and whole wheat bread sandwich," Coste suggests. "Family can help out with this too. When you visit your parents, divide up pumpkin seeds, nuts, blueberries, or already-chopped vegetables into snack size bags and leave them in the refrigerator so they're ready to eat." And talk to your doctor about taking a fiber supplement.This is paragraph text. Double click here to edit and add your own text.
 Omega-3 Fats
Omega-3 Fats
These unsaturated fats, found primarily in fish, have a wide range of benefits, including possibly reducing symptoms in rheumatoid arthritis and slowing the progression of age-related macular degeneration (AMD), a disease of reduced vision in the elderly. "New evidence suggests that omega-3s may also reduce the risk of Alzheimer’s disease and perhaps even keep the brain sharper as we age," says Zelman. Seafood should be part of a heart-healthy diet but omega-3 supplements have not been shown to protect against the heart.
How to hit the mark: Nutrition experts recommend helping yourself to at least two servings of fish a week. Salmon, tuna, sardines, and mackerel are especially high in omega-3 fats. Some vegetable sources of omega 3 include soybeans, walnuts, flaxseed, and canola oil. Omega 3 supplements are available but be sure to talk to your doctor before you begin taking any supplements.
This is paragraph text. Double click here to edit and add your own text.
Water
Water might not seem like an essential vitamin or mineral, but it is crucial for good health. With age, sense of thirst may decline. Certain medicines increase the risk for becoming dehydrated. Water is especially important if you are increasing the fiber in your diet, since it absorbs water. In the Modified MyPyramid for Older Adults, created by Tufts University researchers, 8 glasses of fluids a day are next to physical activity in importance for health.
How to hit the mark: Nutritionists recommend you drink 3 to 5 large glasses of water each day, says Zelman. One sign that you’re drinking enough is the color of your urine. It should be pale yellow. If it is bright or dark yellow, you may need to drink more liquids.
Coste says that adult children can help remind their parents to drink enough water by buying them 4-ounce water bottles. "As we get older, we get overwhelmed really easily," she says. "You open the refrigerator and you see big bottles of water and you close the refrigerator. You see a small bottle of water and you think, 'I can drink that.'"
Some people may need to have their amount of fluids restricted due to medical reasons such as kidney or liver disease. Make sure to check with your healthcare provider about a suitable fluid intake level for you. Taking in too much fluid can be unsafe, too.
Family caregivers play a key role in caring for chronically ill older people. Although neighbors and friends may help, about 80% of help in the home (physical, emotional, social, and economic) is provided by family caregivers. Family caregivers can often delay or even prevent the need for care in residential care facilities.
The amount and type of care provided by family members depend on economic resources, family structure, quality of relationships, and other demands on the family members' time and energy. Some family caregivers provide minimal assistance (for example, periodically checking in) while others provide full-time, complex care. Sometimes care is needed for a short time, as when a person is recovering from surgery. Often, care is needed for months or years. On average, family members caring for older people spend about 4 hours a day in caregiving activities.

Although society tends to view family members as having a responsibility to care for one another, the limits of such obligations vary among cultures, families, and individual family members. The willingness of family members to provide care may be bolstered by supportive services (for example, technical assistance in learning new skills, counseling services, and family mental health services) and supplemental services (for example, personal care such as assistance with grooming, feeding, and dressing, as well as home health care, adult day care, and meals programs). Supplemental services may be provided on a regular schedule or as respite care for a few hours or days. Changes in demographics and social values have reduced the number of family members available to care for impaired older relatives. These changes include the following:
Increased life span: As a result, the population of the very old has been increasing.
Delayed procreation: Combined with increased life span, this delay has created a sandwich generation of caregivers who care simultaneously for their children and their parents. Thus, their children, who are potential caregivers, are likely to be old also.
Increasing mobility of society and the increased divorce rate: Families are more likely to be geographically separated, and family ties may be weakened. Nonetheless, 80% of people 65 or older live within 20 minutes of one child.
An increasing number of women in the workforce: Previously, women may have provided care for older parents, but the demands of a job may diminish or eliminate their ability to do so.
The number of dependent and very sick older people is increasing.
The number of dependent and very sick older people is increasing.
These factors predict an increasing demand for home care services provided by someone other than family members, friends, and neighbors.
Effects
Although caregiving can be very rewarding, it can also have negative effects. Family caregivers may experience considerable stress and subsequent health problems, isolation, fatigue, and frustration, sometimes leading to a sense of helplessness and exhaustion (caregiver burnout) or mistreatment of the older person.
Caregiving may also become a financial burden. Couples in which one partner cares for the other tend to be disproportionately poor. Sometimes a working caregiver needs to leave full-time employment or reduce work hours to accommodate caregiving.
Caregivers can often obtain reassurance or learn helpful information or strategies for caregiving from doctors, nurses, social workers, or case managers. Caregivers can also take the following measures to prepare themselves for caregiving and to avoid caregiver burnout:
Attending to their own physical, emotional, recreational, spiritual, and financial needs
When appropriate, asking for help with caregiving or psychologic support from other family members and friends
Investigating outside groups that can offer psychologic support (such as support groups) or that can help with caregiving (such as counseling, home health care, adult day care, meals programs, and respite care)
Avoiding taking the person's difficult behavior or hostility (if they occur) personally
Last full review/revision November 2016 by Daniel B. Kaplan, PhD, LICSW; Barbara J. B
Rising life expectancy and declining birth rates are resulting in an aging population as well as a widening retirement savings adequacy gap in the ASEAN economies. With the low coverage of mandatory pension schemes and the weakening family-based support for retirement income, the region’s older people are facing serious challenges in maintaining a reasonable standard of living after retirement.
 A recent report by Tsao Foundation’s International Longevity Centre Singapore and Mercer and Marsh & McLennan Companies’ Asia Pacific Risk Center delves into this gap and explores potential solutions to enhance the financial security of women in four ASEAN economies—Indonesia, Malaysia, Singapore and Thailand—and in Hong Kong.
A recent report by Tsao Foundation’s International Longevity Centre Singapore and Mercer and Marsh & McLennan Companies’ Asia Pacific Risk Center delves into this gap and explores potential solutions to enhance the financial security of women in four ASEAN economies—Indonesia, Malaysia, Singapore and Thailand—and in Hong Kong.
With more than half (about 60 percent) of the world’s total population of older persons aged 60 years and over,1 the Asia-Pacific region is poised to become one of the oldest regions in the world, with an estimated 1.3 billion older persons by 2050.
There is also growing recognition of the female face of population ageing. In Asia-Pacific, more than half of all older persons aged 60 years and over are women. Ensuring the financial security of these older women will be one of the major social and economic challenges for the Asia-Pacific region. As Phumzile Mlambo-Ngcuka, UN Under-Secretary General and Executive Director, UN Women underlined, “If not addressed, the feminization of aging has the potential to become one of the biggest challenges to gender equality of this century.
This is paragraph text. Double click here to edit and add your own text.
For older women in the seven countries, employment is not a viable route towards financial security. Fewer older women work compared to older men: in 2015, labor force participation of older women over 65 years was highest in Indonesia (28.7%) and Philippines (27.7%). In part, the lower levels of labor force participation could be due to lower levels of education, a reflection of gender inequalities in access to education earlier in women’s lives.
However, a major factor is women’s greater involvement in caregiving and family responsibilities. Caregiving is not confined to older cohorts of women, but impacts upon women of all ages. Women’s domestic responsibilities are the primary reason for the persistence of the gender gap in labor force participation across all age groups in all the seven countries. In Myanmar, for example, almost half (48%) of women aged 15 years and over were outside the labor force and 64% of these women cited housework and family responsibilities as the main reason for not working.
With family support declining, the need for alternative source of income becomes even more urgent. It is doubtful that income from employment can offset the loss of income from family. Education levels have been steadily rising in all seven countries, which have either achieved or are near gender parity in education, but the gender gap in labor force participation rates remains.
Increasing labor force participation rates would entail a change in the distribution of care work. It is estimated that a decrease in unpaid care work would result in a 10% increase in labor force participation.9 Yet, not only does unpaid care remain a female responsibility, but as societies across Asia are rapidly ageing, the increased pressures for However, a major factor is women’s greater involvement in caregiving and family responsibilities. Caregiving is not confined to older cohorts of women, but impacts upon women of all ages. Women’s domestic responsibilities are the primary reason for the persistence of the gender gap in labor force participation across all age groups in all the seven countries. In Myanmar, for example, almost half (48%) of women aged 15 years and over were outside the labor force and 64% of these women cited housework and family responsibilities as the main reason for not working.
With family support declining, the need for alternative source of income becomes even more urgent. It is doubtful that income from employment can offset the loss of income from family. Education levels have been steadily rising in all seven countries, which have either achieved or are near gender parity in education, but the gender gap in labor force participation rates remains.
Increasing labor force participation rates would entail a change in the distribution of care work. It is estimated that a decrease in unpaid care work would result in a 10% increase in labor force participation.9 Yet, not only does unpaid care remain a female responsibility, but as societies across Asia are rapidly ageing, the increased pressures for caring for the ageing population will only further the need for caregiving.caring for the ageing population will only further the need for caregiving.
The main emphasis of policy should be on addressing these competing trends:
1) Changing the conversation around care: In some of the developing ASEAN countries, the focus should start with young girls and ensuring they remain in school and do not drop out to take care of younger siblings. For women of working age, the key factor will be to ensure they enter and most importantly, remain in the workforce. This would involve a range of measures from the provision of childcare, but critically, to changing the mindset around caregiving responsibilities.
2) Bridging the gap between the ability of families to provide support and actual support provided: Solutions include strengthening community ties, and expanding the scope of non-family support systems such as non-governmental organisations (NGOs).
3) Expanding the reach of social pensions: The role of social protection and in particular, social pensions needs to be explored further.
In addition to the damaging mental effects of feeling that one lacks fulfilling personal relationships, feeling lonely can also take a toll on one’s physical health. A University of California, San Francisco (UCSF) study found that participants 60 years old and older who reported feeling lonely saw a 45 percent increase in their risk of death. Isolated survey respondents also had a 59 percent greater risk of mental and physical decline than their more social counterparts.
This decline manifested specifically in participants’ abilities to perform activities of daily living (ADLs), the six basic tasks that are necessary for truly independent living. In other words, loneliness has the potential to accelerate a senior’s need for assistance from a family caregiver or another source of long-term care.
Loneliness is thought to act on the body in a way that is similar to chronic stress. It raises the levels of stress hormones like cortisol in the body, which impairs immune responses and contributes to inflammation, mental illness and conditions like heart disease and diabetes. Another study published in the Journal of the American Medical Association
Psychiatry even found that loneliness may be associated with the development of brain biomarkers associated with preclinical Alzheimer’s disease.
Even when a senior is being taken care of by family caregivers, T. Byram Karasu, MD, from the department of psychiatry and behavioral sciences at the Albert Einstein College of Medicine, says that there is often little attention paid to deep, engaging communication between a senior and the rest of the family. The changes listed above are factors, but caregivers are usually so worn out from juggling their day-to-day responsibilities that they have little time or energy left for truly meeting a senior’s emotional and social needs.
Bobbie Smith, a professional caregiver for Home Instead Senior Care with more than six decades of elder care experience under her belt, echoes this sentiment but believes the issue actually runs deeper throughout the structure of families. She says that a modern trend is the breakdown of extended family relationships—like those between grandparents and grandchildren.
This has caused many elderly people to feel as though they have been “pushed to the side” and forgotten about. This is especially true for family units that have spread across the country and have difficulty making time for visits and even regular communication by phone and mail.
Age brings many difficult changes that contribute to a more solitary life. One of the biggest issues for seniors is that their social circles begin to shrink as the years go by. Friends, significant others and family members move away or pass away. Even those who still live close by may be inaccessible due to limited mobility, especially once a senior can no longer drive safely. Age-related changes in one’s physical condition, such as hearing loss and low vision, can make it so difficult to communicate that it doesn’t seem worth the effort anymore.
Embarrassment can be a factor as well. Many older adults who suffer from incontinence, are on oxygen therapy or need to use a mobility aid to get around not only face logistical obstacles when it comes to leaving the house, but they must also overcome feeling self-conscious about these “obvious” signs of aging.
It is trying enough for a senior to maintain healthy relationships despite these challenges, but when one’s entire peer group is experiencing any combination of these factors, it can be difficult if not impossible to get together or keep in touch on a regular basis. Sadly, many seniors experience a decline in the number and quality of their relationships as they age, whether it is self-imposed or due to outside forces.
We live in an age where we can communicate with friends and family members across the country and around the globe with a few clicks of a mouse or taps on a smart phone screen. However, despite advances in communications technology and the increasing connectedness it brings, research indicates that, as a society, we are lonelier than we have ever been. Perhaps no other age group feels the keen sting of loneliness more than the elderly.
 Lastly, psychologists from the University of Chicago analyzed data from an ongoing multi-generational cardiovascular study that began in 1948 and discovered another remarkable characteristic of loneliness: It is contagious. Older adults who feel lonesome are more prone to behave in ways that may cause other people to not want to be around them. Researchers found that solitary seniors have a tendency to further isolate themselves by pushing people away and not making efforts to engage with others. Furthermore, the few people that lonely seniors interact with are likely to become lonely themselves and follow the same path to the outskirts of their social networks. This has serious implications on the health and social lives of family members who are caring for lonely seniors.
Lastly, psychologists from the University of Chicago analyzed data from an ongoing multi-generational cardiovascular study that began in 1948 and discovered another remarkable characteristic of loneliness: It is contagious. Older adults who feel lonesome are more prone to behave in ways that may cause other people to not want to be around them. Researchers found that solitary seniors have a tendency to further isolate themselves by pushing people away and not making efforts to engage with others. Furthermore, the few people that lonely seniors interact with are likely to become lonely themselves and follow the same path to the outskirts of their social networks. This has serious implications on the health and social lives of family members who are caring for lonely seniors.
This is paragraph text. Double click here to edit and add your own text.
•Listen and observe. “We often don’t listen enough to the people we love,” laments Tina Tessina, PhD, psychotherapist and author of The Ten Smartest Decisions a Woman Can Make After Forty. According to Tessina, “Saying ‘tell me more’ is a gift you can give from your heart.” Encouraging them to express themselves can help you discover what interests and passions lay dormant, just waiting to be rekindled.
“You’ve got to really dig deep and find out what their interests were before and get them to try and awaken those forgotten activities,” Smith says. Keep in mind that once-loved activities may no longer interest them or fit their abilities. Do your best to help them discover ways to adapt these hobbies or find new pastimes altogether.
Develop a strategy to defeat seclusion. Once you know what your loved one enjoys doing, you can use this information to develop a personalized loneliness eradication plan. For example, while Smith was caring for an angry 91-year-old man who was reluctant to communicate, she discovered that he had a passion for singing and photography. One day while walking down the hall with him, she began to belt out a few bars of Let Me Call You Sweetheart. The man responded by singing right along with her and grudgingly admitting, “You’re OK.” Today, he sings for his community and is part of a club of retired photographers that Smith helped him contact. Sometimes our elders just need a creative push to step outside their comfort zone.
 Let them teach you. Smith encourages caregivers to connect with their loved ones by allowing them to pass some hard-earned knowledge on to you. “I learn something new every day because I am being taught by the best,” Smith admits. The key is to let the senior’s passions and experiences guide the lesson plan. For example, if your mother loves to embroider, ask her to teach you how to do it. This not only has the potential to be a great bonding experience, but it can also help restore a bit of balance to the child-parent dynamic that may have been lost once caregiving began.
Let them teach you. Smith encourages caregivers to connect with their loved ones by allowing them to pass some hard-earned knowledge on to you. “I learn something new every day because I am being taught by the best,” Smith admits. The key is to let the senior’s passions and experiences guide the lesson plan. For example, if your mother loves to embroider, ask her to teach you how to do it. This not only has the potential to be a great bonding experience, but it can also help restore a bit of balance to the child-parent dynamic that may have been lost once caregiving began.
Bridge the generation gap. According to Smith, caregivers can play a vital role in fostering a relationship between a senior and their youngest relatives. Grandkids often see their grandparents as either crazy or boring, when they should consider their elders sources of valuable wisdom and fun. Try to come up with ways to help the oldest and the youngest generations of your family spend time together, whether in person, by phone or via mail.
Karasu also points out that seniors have the potential to contribute a lot to their families if they are allowed to remain engaged. He says this is doubly important, considering research has shown that an unengaged elderly adult will experience cognitive decline at a much faster rate than a senior who is mentally stimulated by interactions with other people.
 It’s the thought that counts. Another piece of advice from the pros is to urge other family members to reach out to an elderly loved one. It doesn’t have to be a grand, time-consuming gesture. Something as simple as sending a card, sharing a favorite meal, or calling for 30 minutes a couple times a week can go a long way to making a senior feel loved and connected to the rest of the family.
It’s the thought that counts. Another piece of advice from the pros is to urge other family members to reach out to an elderly loved one. It doesn’t have to be a grand, time-consuming gesture. Something as simple as sending a card, sharing a favorite meal, or calling for 30 minutes a couple times a week can go a long way to making a senior feel loved and connected to the rest of the family.
This is paragraph text. Double click here to edit and add your own text.
Consider senior living. For some seniors, no amount of effort encourages them to come out of their shell. It may take a large change to get them to reignite their interest in people and activities. While placement in a senior living community or a long-term care facility might seem like a viable solution for a lonely elder, it isn’t always that straightforward.
The success of such a transition depends on the individual person and the fit of the facility. It also takes time and effort for a loved one to adapt to and grow comfortable with their new living arrangement and neighbors. In fact, it may appear to backfire at first. “When seniors move to nursing homes, assisted living communities, etc., it can be a totally disorienting experience,” Dr. Karasu points out. Family members and staff should provide gentle encouragement to help new residents acclimate, meet new people and participate in activities and events. One of the best parts of senior living (aside from receiving necessary care) is that opportunities for socialization and fulfillment are available right outside a resident’s bedroom door.
STEP ONE – GET A CAPTIVE AUDIENCE
Professional financial predators must first get a captive audience of willing seniors together. Watch out for the “Free Lunch” or “Free Seminar” where you are promised free and important information on “Living Trusts” or “Reverse Mortgages.”Professional financial predators must first get a captive audience of willing seniors together. Watch out for the “Free Lunch” or “Free Seminar” where you are promised free and important information on “Living Trusts” or “Reverse Mortgages.”Professional financial predators must first get a captive audience of willing seniors together. Watch out for the “Free Lunch” or “Free Seminar” where you are promised free and important information on “Living Trusts” or “Reverse Mortgages.”
STEP TWO – FIND OUT WHAT THE SENIOR OWNS
The next step is to find out what the senior owns in terms of
property, savings, annuities, equity in home and other assets.
This is accomplished by handing out questionnaires at the
“Free Lunch” or “Free Seminar” that will be used to determine
which attendees will later be targeted for financial exploitation
at a sales presentation.
STEP THREE – CREATE A NEED TO MOVE THE ASSETS
The financial predator needs to create a need for the senior to move his or her assets or buy and expensive insurance product, like an annuity that pays the predator a huge commission. This is usually accomplished by creating fear and insecurity about one’s life savings. The scammer will tell you he will “protect your estate” and “secure it for your children,” You might be told that “you will go into a nursing home and outlive your money,” or need to “avoid probate,” or “qualify for Medi Cal,” or a host of other doom and gloom scenarios to create enough fear and concern to induce you to comply with the predator’s wishes.
• STEP FOUR – LIQUIDATE THE
SENIOR’S ASSETS AND MOVE
THEM TO COMMISSION-BASED
PRODUCTS
The final step is to close the deal by having the senior move his or her money somewhere where the predator earns a commission. Watch out for IRA Rollovers, Direct Cash Purchases, Reverse Mortgages, Consulting Fees for Assistance in Qualify for a Government Product, or the purchase of an Expensive Annuity. All of these transactions can be used for an inappropriate and unsuitable purpose.
Therapeutic Ultrasound
Publishing in Science Translational Medicine, the team describes the technique as using a particular type of ultrasound called a focused therapeutic ultrasound, which non-invasively beams sound waves into the brain tissue. By oscillating super-fast, these sound waves are able to gently open up the blood-brain barrier, which is a layer that protects the brain against bacteria, and stimulate the brain’s microglial cells to activate. Microglial cells are basically waste-removal cells, so they’re able to clear out the toxic beta-amyloid clumps that are responsible for the worst symptoms of Alzheimer’s.
Many elderly adults are abused in their own homes, in relatives’ homes, and even in facilities responsible for their care. If you suspect that an elderly person is at risk from a neglectful or overwhelmed caregiver, or being preyed upon financially, it’s important to speak up. Everyone deserves to live in safety, with dignity and respect. Learn about the warning signs of elder abuse, what the risk factors are, and how you can prevent and report the problem.
What is elder abuse and neglect?
Elder abuse includes physical, emotional, or sexual harm inflicted upon an older adult, their financial exploitation, or neglect of their welfare by people who are directly responsible for their care. In the U.S. alone, more than half a million reports of elder abuse reach authorities every year, and millions more cases go unreported.
As older adults become more physically frail, they’re less able to take care of themselves, stand up to bullying, or fight back if attacked. Mental or physical ailments can make them more trying companions for those who live with them. And they may not see or hear as well or think as clearly as they used to, leaving openings for unscrupulous people to take advantage of them.
Elder abuse tends to take place where the senior lives: where their abusers are often adult children, other family members such as grandchildren, or a spouse or partner. Elder abuse can also occur in institutional settings, especially long-term care facilities.
Types of elder abuse
Abuse of elders takes many different forms, some involving intimidation or threats against the elderly, some involving neglect, and others involving financial trickery. The most common are:
Physical elder abuse – The non-accidental use of force against an elderly person that results in physical pain, injury, or impairment. Such abuse includes not only physical assaults such as hitting or shoving but the inappropriate use of drugs, restraints, or confinement.
Emotional elder abuse – The treatment of an older adult in ways that cause emotional or psychological pain or distress, including:
• Intimidation through yelling or threats
• Humiliation and ridicule
• Habitual blaming or scapegoating
• Ignoring the elderly person
• Isolating an elder from friends or activities
• Terrorizing or menacing the elderly person
Sexual elder abuse – Contact with an elderly person without their consent. Such contact can involve physical sex acts, but activities such as showing an elderly person pornographic material, forcing the person to watch sex acts, or forcing the elder to undress are also considered sexual elder abuse
Elder neglect – Failure to fulfill a caretaking obligation. This constitutes more than half of all reported cases of elder abuse. It can be intentional or unintentional, based on factors such as ignorance or denial that an elderly charge needs as much care as they do.
Financial exploitation – The unauthorized use of an elderly person’s funds or property, either by a caregiver or an outside scam artist. An unscrupulous caregiver might:
• Misuse an elder’s personal checks, credit cards, or accounts
• Steal cash, income checks, or household goods
• Forge the elder’s signature
• Engage in identity theft
Typical scams that target elders include:
• Announcement of a “prize” that the elderly
person has won but must pay money to claim
• Phony charities
• Investment fraud
Healthcare fraud and abuse – Carried out by unethical doctors, nurses, hospital personnel, and other professional care providers. This can include:
• Not providing healthcare, but charging for it
• Overcharging or double-billing for medical care or services
• Getting kickbacks for referrals to other providers or for prescribing certain drugs
• Overmedicating or undermedicating
• Recommending fraudulent remedies for illnesses or other medical conditions
• Medicaid fraud
Elder self-neglect
One of the most common forms of elder abuse encountered by geriatric care managers is self-neglect. Physical or mental impairment or diminished capacity can mean that an older adult is no longer able to perform essential self-care. They may lack basic personal hygiene, appear dehydrated, malnourished, or underweight, live in increasingly unsanitary or dirty conditions, and be unable to pay bills or properly manage their medications.
Self-neglect can be a sign of depression, grief, dementia, or other medical problem, and in many cases, the older person will refuse to seek assistance. They may be in denial, feel ashamed about needing help, or worried about losing their independence.
Warning signs of elder abuse
Signs of elder abuse can be difficult to recognize or mistaken for symptoms of dementia or the elderly person’s frailty—or caregivers may explain them to you that way. In fact, many of the signs and symptoms of elder abuse do overlap with symptoms of mental deterioration, but that doesn’t mean you should dismiss them on the caregiver’s say-so.
Frequent arguments or tension between the caregiver and the elderly person or changes in the personality or behavior in the elder can be broad signals of elder abuse. If you suspect abuse, but aren’t sure, you can look for clusters of the following warning signs.
Physical abuse warning signs:
• Unexplained signs of injury, such as bruises, welts, or scars, especially if they appear symmetrically on two sides of the body
• Broken bones, sprains, or dislocations
• A report of drug overdose or an apparent failure to take medication regularly (a prescription has more remaining than it should)
• Broken eyeglasses or frames
• Signs of being restrained, such as rope marks on wrists
• Caregiver’s refusal to allow you to see the elder alone
Emotional abuse warning signs:
• Threatening, belittling, or controlling caregiver behavior
• Behavior from the elder that mimics dementia, such as rocking, sucking, or mumbling to themselves
Sexual abuse warning signs:
• Bruises around breasts or genitals
• Unexplained vaginal or anal bleeding
• Torn, stained, or bloody underclothing
Elder neglect or self-neglect warning signs:
• Unusual weight loss, malnutrition, dehydration
• Untreated physical problems, such as bed sores
• Unsanitary living conditions: dirt, bugs, soiled bedding and clothes
• Being left dirty or unbathed
• Unsuitable clothing or covering for the weather
• Unsafe living conditions (no heat or running water; faulty electrical wiring; other fire hazards)
• Desertion of the elder at a public place

Financial exploitation warning signs:
• Significant withdrawals from the elder’s accounts
• Sudden changes in the elder’s financial condition
• Items or cash missing from the senior’s household
• Suspicious changes in wills, power of attorney, titles, and policies
• Addition of names to the senior’s signature card
• Financial activity the senior couldn’t have undertaken, such as an ATM withdrawal when the account holder is bedridden
• Unnecessary services, goods, or subscriptions
Healthcare fraud or abuse warning signs
• Duplicate billings for the same medical service or device
• Evidence of overmedication or under-medication
• Evidence of inadequate care when bills are paid in full
• Problems with the care facility: poorly trained, poorly paid, or insufficient staff; crowding; inadequate responses to questions about care
Risk factors for elder abuse
It’s difficult to take care of a senior who has many different needs, and it’s difficult to be elderly when age brings with it infirmities and dependence. Both the demands of caregiving and the needs of the elder can create situations in which abuse is more likely to occur.
Many nonprofessional caregivers—spouses, adult
children, other relatives and friends—find taking care of
an elder to be satisfying and enriching. But the
responsibilities and demands of caregiving, which
escalate as the elder’s condition deteriorates, can also
cause significant stress. The stress of elder care can
lead to mental and physical health problems that leave
caregivers burned out, impatient, and more susceptible to
neglecting or lashing out at the elders in their care.
In addition to the caregiver’s inability to manage stress, other risk factors for elder abuse include:
• Depression in the caregiver
• Lack of support from other potential caregivers
• The caregiver’s perception that taking care of
the elder is burdensome and without emotional
reward
• Substance abuse by the caregiver
• The intensity of the elderly person’s illness or dementia
• Social isolation—the elder and caregiver are alone together almost all the time
• The elder’s role, at an earlier time, as an abusive parent or spouse
• A history of domestic violence in the home
• The elder’s own tendency toward verbal or physical aggression
Even caregivers in institutional settings can experience stress at levels that lead to elder abuse. Nursing home staff may be prone to elder abuse if they lack training, have too many responsibilities, are unsuited to caregiving, or work under poor conditions.
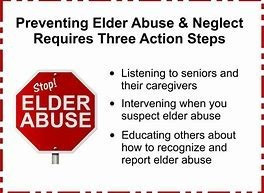
Preventing elder abuse and neglect
If you’re a caregiver to an elderly person and feel you are in danger of hurting or neglecting them, help and support are available. Perhaps you’re having trouble controlling your anger and find yourself screaming louder and louder or lashing out at the person in your care? Or other people have expressed concern with your behavior or the tension between the two of you? Or maybe you simply feel emotionally disconnected or overwhelmed by the daily needs of the elderly person in your care? Recognizing that you have a problem is the biggest step to getting help and preventing abuse.
As a caregiver, the following steps can help you prevent elder abuse or neglect:
Take immediate steps to relieve stress and burnout. Stress is a major contributor to elder abuse and neglect. You can help reduce your stress levels by regularly practicing stress-relieving techniques such as yoga, meditation, or deep breathing exercises.
Request help from friends, relatives, or local respite care agencies or find an adult daycare program. Every caregiver needs to take regular breaks from the stress of caring for an elder and to attend to their own needs, if only for a couple of hours.
Learn techniques for getting your anger under control.
Take care of yourself. If you are not getting enough rest, you are much more likely to succumb to anger. Eat a healthy diet, get regular exercise, and take care of your own medical needs.
Seek help for depression. Family caregivers are especially at
risk for depression, but there are plenty of things you can do to
boost your mood and outlook and overcome the problem.
Find a support group for caregivers of the elderly. Sharing
your concerns and experiences with others facing the same
challenges can help relieve the isolation you may be feeling as a caregiver. It can also be a great place to gain valuable tips and insight into caring for an elder.
Get help for any substance abuse issues. It’s never easy, but there are plenty of actions you can take to address drug or alcohol abuse.
Get professional help. If you can’t seem to stop yourself no matter how hard you try, it’s time to get help by talking to a therapist.
If you’re a concerned friend or family member, the following can also help to prevent abuse of an elderly person.
Call and visit as often as you can, helping the elder to see you as a trusted confidante.
Offer to stay with the elder so the caregiver can have a break—on a regular basis, if possible.
Monitor the elder’s medications to ensure the amounts being taken correspond with the prescription dates.
Watch for financial abuse by asking the elder if you can check their bank accounts and credit card statements for unauthorized transactions.
Identify the warning signs of abuse or neglect and report it without delay.
How to protect yourself from abuse as an elder
• Make sure your financial and legal affairs are in order. If they aren’t, enlist professional help to get them in order, with the assistance of a trusted friend or relative if necessary.
• Keep in touch with family and friends and avoid becoming isolated.
• If you are unhappy with the care you’re receiving, whether it’s in your own home or in a care facility, speak up. Tell someone you trust or call an elder abuse helpline.
Reporting elder abuse
If you are an elder who is being abused, neglected, or exploited, tell at least one person. Tell your doctor, a friend, or a family member whom you trust. Or call one of the helplines listed below. If you see an older adult being abused or neglected, don’t hesitate to report the situation. And if you see future incidences of abuse, continue to call and report them. Each elder abuse report is a snapshot of what is taking place. The more information that you can provide, the better the chance the elder has of getting the quality of care they need. Older adults can become increasingly isolated from society and, with no work to attend, it can be easy for abuse cases Many seniors don’t report the abuse they face even if they’re able. Some fear retaliation from the abuser, while others view having an abusive caretaker as better than having no caretaker and being forced to move out of their own home. When the caregivers are their children, they may feel ashamed that their children are inflicting harm or blame themselves: “If I’d been a better parent when they were younger, this wouldn’t be happening.” Or they just may not want children they love to get into trouble with the law. In any situation of elder abuse, it can be a real challenge to respect an older adult’s right to autonomy while at the same time making sure they are properly cared for.
In the case of an elder experiencing abuse by a primary caregiver, such as an adult child:
Do not confront the abuser yourself. This may put the older person in more danger unless you have the elder’s permission and are able to immediately move them to alternative, safe care.
Find strength in numbers. If a family caregiver is suspected of abuse, other family members may have the best chance of convincing the older adult to consider alternative care.
Feelings of shame can often keep elder abuse hidden. You may not want to believe a family member could be capable of abusing a loved one, or you may even think that the older adult would be angry at you for speaking up. But the earlier you intervene in a situation of elder abuse, the better the outcome will be for everyone involved.
In the case of self-neglect:
Even if the elder refuses your help, keep checking in with them.
Enlist others to express their feelings of concern to them. Sometimes a peer or a neutral party, such as a geriatric care manager, may have a better chance of getting through.
Make sure the older adult is connected with medical services. Since self-neglect can have medical causes, share your concerns with the elder’s doctor if possible.
Offer the elder home services on a trial basis. This can help them see the positive changes they can experience, and open them up to considering alternative care. For example, encourage them to try housekeeping help for a month or a meal delivery service for a few weeks.
Tour assisted living or other senior housing facilities without any immediate pressure to move. This may help dispel any myths or eradicate the older person’s fears about moving.
Consider legal guardianship. If you are concerned that a person’s ability to take care of themselves safely is compromised, you can look into legal guardianship or legal conservatorship. If there is not an appropriate family member available, a guardian can be appointed by the court.
By: Walt Pickut
Updated August 14, 2017, www.pocketsense.com
You might be called elderly if you are older than 60, by some definitions, and your physical abilities might start limiting your freedom to go where you want to go when you want to go there. For instance, according to a 2011 report by statisticians at Caregivers Library, there are 8.4 million seniors in the United States who depend on other people for transportation. Many transportation problems can be solved with common sense solutions.
How to protect yourself from abuse as an elder
• Make sure your financial and legal affairs are in order. If they aren’t, enlist professional help to get them in order, with the assistance of a trusted friend or relative if necessary.
• Keep in touch with family and friends and avoid becoming isolated.
• If you are unhappy with the care you’re receiving, whether it’s in your own home or in a care facility, speak up. Tell someone you trust or call an elder abuse helpline.
Driving Problems
Cars and roadways are built for the average driver's reflexes, agility and vision. But, as pointed out by Caregivers Library, aging drivers eventually lose the ability to use these transportation systems as they are designed. The size of sign wordage, distance from warnings to hazards, size and brightness of lighted signals and many other features make roads less accommodating to elderly drivers.

Distance To Public Transportation
Studies published in the "Japanese Journal of Gerontology" document the ongoing problem for elderly non-drivers of walking distance to public transportation systems. Bus routes to elder care facilities might help, but, especially in rural areas where public transportation might be inaccessible, isolation also can limit access to taxis or other services for transportation.
Inadequate Ingress
Public transportation, for instance buses and trains, might require an inconveniently high step for entry. "Kneeling" buses or extendible steps can help. Transportation stations also can present turnstile obstacles.
Timing
Subway cars usually are at platform levels but the duration of door opening might be too brief for slow walkers. If an elderly person chooses to walk, traffic signal timing might present a problem if a green light is too brief to permit safe crossing, as documented in the Japanese studies.
Steps Vs. Ramps
Most municipalities require wheelchair ramp access to street crossings, public buildings and public transportation stations. But old construction, which limits ramp space, and budget constraints make this solution less than universal.
Scheduling
The Japanese researchers detected significant differences between the hours elderly people want transportation and the hours mass transport might be most available. To avoid heavy sidewalk traffic, for instance when going to and from bus stations, many elderly avoid rush hours, but public systems often decrease service during off hours.

Geography and Poverty
Inability to drive, the most common elderly transportation problem, makes geography problematic. In the absence of door-to-door assistance by other drivers, elderly people might be stopped even by low hills that are irrelevant to younger people. Urban and rural isolation and inability to pay for multiple modes of transportation can make the elderly into virtual prisoners in their homes.
Fragmented Services
In a report to Congress presented by the U.S. Government Accounting Service, a special problem for elderly travelers is identified as fragmentation or dis-coordination among transportation services. Failure to coordinate pickup and drop-off routes and schedules, travel fares, accessibility barriers and other issues continue to be problems.
This is paragraph text. Double click here to edit and add your own text.
Burden To Others
The Japanese gerontology researchers identified one transportation problem as self-imposed: Many elderly people, realizing that their need for help increases over time, resist becoming a burden to family and friends. Strong family support, churches and civic groups are identified as potential solutions.
Family Conflict
While daily travel by the elderly might decrease with age, it also might increase with greater medical care travel needs. Simultaneously, transportation needs of their children's growing families and complex schedules might increase over time. Family might become unable, unwilling or impatient with the transportation problems of their elderly members.
That’s the first thing people ask me after I tell them I
develop programs that teach seniors technology at Brookdale
Senior Living. In today’s increasingly digital world, many visits
with parents or grandparents are punctuated with questions
about technology. I was reminded of this just last week when
visiting my own grandmother at a Brookdale community in
California. After spending nearly an hour searching for her
current Gmail and Apple ID passwords, we realized that my
grandmother’s iPad wasn’t even connected to WiFi!
You’ve likely been through a similar routine if you have a new tech inquisitive senior in your life. Before your next visit, consider arming yourself with the following 10 tips. You’ve likely been through a similar routine if you have a new tech inquisitive senior in your life. Before your next visit, consider arming yourself with the following 10 tips for teaching technology to seniors. for teaching technology to seniors.
1. When introducing new tech concepts, build on existing knowledge. Comparing a new technology concept with something the senior is already familiar with will make it easier for them to understand. When we introduce web browsing in Brookdale’s tech programming, we compare web addresses to street addresses. This helps reinforce the idea of web navigation in a way that is intuitive to our residents because they can think of it like navigating a row of buildings.
2. Explain the relevance before going into detail.. Before launching into the mechanics of how to use today’s trending gadget, explain how the senior might benefit from using it. If you’re introducing someone to Facebook, start by showing them pictures of their grandchildren they might not have seen. Once they see how easily accessible the pictures are, they’ll be more patient with the process of setting up an account and exploring their newsfeed.
3. Avoid technical words and use consistent language. Now that words like emoji and selfie have been added to Oxford Dictionary’s lexicon, tech speak is becoming a part of everyday language. As you talk tech with seniors, be mindful of the words you use. Many tech-related terms may be unfamiliar to them. When there are multiple terms that can be used to describe something, choose the simplest option and be consistent.
4. Watch your pace. This may seem obvious, but it’s important to remind yourself not to move too quickly when introducing a senior to technology. Pause between each step to give them a moment to process what they’ve just learned. If you’re not sure whether or not you are moving too quickly, ask the senior how they are feeling about the pace.
5. Repeat key concepts. The sheer volume of new information they are taking in can easily overwhelm seniors learning technology for the first time. Repeating key concepts will make them easier to remember and will reinforce the most important takeaways.
6. Build in regular time to ask questions. Be sure to build in regular time for questions before moving to new concepts. Some seniors may be reticent to interject with a question. Providing a specific moment where questions are expected may help make them feel more comfortable. It will also give you an idea of what concepts you need to spend extra time on.
7. Let the resident actively practice the new tech skills. When watching a senior struggle to navigate on their device it may be tempting to take matters into your own hands, but the time saved in the short term will not yield good learning results. Seniors need to take an active role as they learn new technology so they can become accustomed to the tactile nuances involved in tapping, clicking and button pressing.
8. Direct them to senior specific tech resources. Encourage the senior to utilize tech resources for seniors between your visits. If
they live in a Brookdale community, speak with the
Resident Programs Leader and ask about
Brookdale’s iPad Program and any other regularly
scheduled tech activities. Be sure they know how to
access resources available online such as
TechBoomers and AARPTek which offer excellent
free tech tutorials designed specifically for seniors.
9 Validate expressions of confusion, but reinforce that they can and will learn. Seniors are used to being more knowledgeable and competent at most of their endeavors by virtue of the fact that they have more life experience. It may have been years since they were a novice at something, so when they express frustration, be sure to validate the difficulty of learning technology for the first time. Reinforce that learning something new is always hard but that with practice they will advance. It may also help to share any difficulties or confusion you’ve experienced when learning technology in the past.
10. Seek Out Wow Moments. For everyday technology users, it’s easy to forget just how amazing technology really is. Be sure to create opportunities for technology to wow the senior, like showing them their childhood home on Google Earth or FaceTiming with a close friend they haven’t seen in years. The more they see the incredible things technology enables them to do, the more they will engage with it which will make mastering it a breeze.
1. Test makeup in the right places
Swipe lipstick on your thumb and foundation, concealer and shadow in the web between thumb and forefinger. No more wiping clean the store tester and applying to your face or the back of your hand, please. Not only is it unhygienic, it’s not realistic. Test on skin similar to the area where the product will be used. The soft, fleshy blue-red pad of your thumb is more like actual lip skin and gives a truer idea of lipstick shade and texture. The web of skin near your thumb is thinner, looser and crinkled — it will show how face makeup or eye shadow will look when applied, blended and worn.
2. Apply skin care upward and outward
It really does help counteract gravity, and it sidekicks saggy skin and deep expression lines. Blend on creams, serums and oils in gentle sweeping movements, working from the center of your face outward. In the short term, it gets the circulation going, helps products melt into skin and feels soothing — in the long term, it minimizes the downward pull. Makeup artists, day spa aestheticians, facialists and the teeny print instructions sheet that comes with luxury face creams wouldn’t have it any other way! Start at the base of your neck and work upwards to the jawline. Then sweep outward along the jawline, from chin to ears, beneath nose to cheekbones to temples, in a big C. Blend eye cream from inner eye near the nose, in a hammock following the under eye. You’re subtly lifting the face as you massage up and out.
3. Apply brow makeup before eye makeup, not after
Unless you have tattooed or microbladed your eyebrows, or have genetically gifted strong full brows — your own are not what they used to be. Filling and extending your brow shape before jumping to liner, shadow and mascara gives your eye area a brand-new bigger frame. This “window” will affect how much eye makeup you need or want — and maybe it's not as much as you thought. Dark hair? Go one or two shades lighter in brow makeup. Light hair? Go one or two shades darker in brow filler.
4. Start and stop brow makeup where it should.
Improving or inventing mature brows is a biggie, but we often pay too much attention to fullness and shape, not length. This is why even “corrected” brows fall short. Line up any pencil vertically from the outside corner of your nose to align with your inner eye corner. This is where your brow should begin. Fill in your brow with small, hair-like, upward pencil strokes, then angle the pencil from the nose to the outer corner of your eye. This is where your brow should end. Warning: Do not follow the downward curve of brow hairs that droop. Instead, cheat the line outward for a straighter look, and pluck hairs that drag your eye down. Comb brow hairs up, and fill from the bottom to top with pencil and/or powder.
5. Our faces become more asymmetrical with age. Don’t fight it.
By age 50, unmatched features are the norm. One brow may be higher or differently shaped than the other; your top lip may have thinned to a nearly invisible line, while the bottom lip is still pouty. On your face, you may see that one side is more lined and crinkled than the other (usually the side you don’t sleep on is higher, firmer, less lined). It’s all OK. These quirky little “off” things give your face personality and individuality. Don’t strive to mask differences with makeup.
6. A makeup sponge is for adding moisture, not makeup.
Here’s a major secret: Unlike fingers, makeup sponges suck up a lot of face makeup. You end up using more makeup for each application and running out of that bottle or tube very quickly. The more expensive teardrop sponge is trendy, but those triangular ones have been around forever and do the job just as well. Use them to freshen a makeup overdose or retouch makeup during the day or evening. Simply run a makeup sponge under warm water, squeeze out the excess and dab (press, don’t swipe!) your face right over your makeup. It removes any excess color (too much foundation, blush or bronzer, for example) or makeup that has settled in crevices and lines. Carry one in a Ziploc bag in your handbag, and clean it often.
7. Create a new eyelid crease
Aging eyes are beautiful, but when deep, hooded or saggy, they rob your lids of space. This puts the emphasis on the droopy overhang and diminishes eye size and shape. When applying makeup forget the old rules about using a light shadow on the lid and a deeper color to contour. Instead, go darker on the lids with a medium shade (anything from gray to light brown), and blend it from the lash line straight up and over your real crease to extend above it. Keep the edge of the arc soft. This new fake crease is an illusion that expands lash to crease space, pushes back the overhang and makes eyes look bigger and stronger in shape — even before you get to liner!
8. Work your eye liner strategically.
Stop applying liner on autopilot. Vary placement and line thickness according to a specific goal — and this may differ daily. You can, for example: rim upper and lower lids to really emphasize eye shape and draw attention away from underage bags or lines; line the upper lid at the lash roots and beneath them in the waterline to bring deepest eyes out; widen the top lid liner slightly at the outer end to lift the eyes; use a gray or brown liner instead of dark, inky black or chocolate for a softer look; line the lower waterline with a beige eye pencil to cancel out redness. The options are endless.
9. The center of your face is where you need the most coverage.
Stop obsessing about those cheeky brown spots — no one else is even noticing them. Start at your nose (bridge to beneath nostrils) and its surrounding area, since this is where redness, dark circles, broken capillaries, enlarged pores require coverage. Apply foundation or your beauty balm/color-correcting (BB/CC) cream in the center, and blend outward from there toward hairline, jaw and ears, sheering the texture as you go. Then for round two, go over the area again, using a foundation brush in a back-and-forth motion every which way, like painting a wall. This forces the makeup and skin to melt together seamlessly instead of lying on top. Aim for subtle coverage with skin visible beneath.
10. Manipulate your same old lipstick’s texture and shade
You already know lining and filling in lips with a lip-toned pencil will prevent ring around the mouth and hold the color, but you don’t know this: You can turn any lipstick into a more matte or muted one by blotting with a tissue and satin or matte powder — select from pressed to loose, even blush, a peachy, rosy, tawny eyeshadow or bronzer — any kind works. This tip softens the look of too bold bright or deep berry shades, too. Want more shimmer or shine that won’t get sloppy and slimy? Apply your usual lipstick and dab it with a glittery, shimmery powder as above.
is
Cartoonish brows.
Worse than the sparse arch is a harsh, overdone brow. The culprit may be the wrong tool, like an eyeliner pencil that is soft and goes on too strong. A brow pencil is designed to be hard and go on softly, so your brows look natural,
OD'ing on foundation.
As hormone levels dip and your skin gets drier, you may reach for a cream foundation. Not so fast: Thicker, creamier formulas are usually made to provide fuller coverage, which means they're packed with more pigment. And pigment is basically powder. If you like a creamy formula's coverage, try it with a richer face moisturizer or a hydrating primer
Foundation that's too pale.
Skin grows more pallid with age, so if you're wearing a matchy-matchy foundation, it can leave you looking pasty. (Yep, time to ditch the rule that says you should match.) Put life back into your skin with a slightly warmer tone. You can also just mix an exact-match shade with the next darkest hue on the back of your hand, and then apply with a foundation brush.
Caked-on concealer.
As soon as you've reached the years when you really need a concealer, it can let you down by sinking into lines. To keep concealer from drawing attention to wrinkles, apply it only on the inner halves of your under-eyes to cover up any darkness. Or just skip the concealer and use a brush-on highlighter pen.
Streaky blush.
Forget stroking blush from mouth to ear; that technique only emphasizes gauntness as you get older. An instant trick to lift cheeks: Swirl blush ever so slightly higher on the apples.
Highlighter everywhere.
Avoid a cartoonish look and only brush your highlighter in specific, face-flattering areas. Wearing highlighter in the wrong place can give you the opposite of a luminous effect. Use it where the light naturally touches your face, like the brow bone, bridge of the nose and along the cheekbones.
Overdone eyes.
Oily lids can spell ruin for eyeshadow, but piling on extra will only make your eyes look weighed down. Your best bet: First apply a thin layer of a clear primer.
Muddy eyeshadow.
If brown and bone are your go-to eyeshadows, take note: Brown has yellow or red pigments in it, either of which can actually make eyes look tired. Also be careful with once-"safe" shadows like bone; they're often too light to cover discoloration on lids. Your new go-tos: sage and jewel tones.
Jagged, uneven liner.
Avoid tugging at the outer corners of your eyes. This can cause skin to crinkle, and your line will not be as smooth." Instead, point your chin up and look down, so your lids are half-closed but you can still see them, and use a liquid liner.
Droopy lashes.
Lashes can make eyes look more youthful and awake, but one common mistake is skipping the eyelash curler. Use it to curl each lash at the root, holding for 15 seconds.
Wearing the same old lip colors.
It's the easiest way to refresh your look. If you've been wearing neutrals since the '90s, try red. If you've been loyal to red, try a pink. Play with the color, but go easy on texture. Anything that's severe — a lipstick or hairdo — will age you. So wear a red, but a sheer one.
Lipstick that bleeds.
Extra lipstick migrates, especially as the definition of the lip's border softens with age. So, instead of applying color straight from the tube, apply with a lipstick brush. Dab on the center of your lips, and then spread it to the corners.